FRACTURE
OVERVIEW
- Fracture is the break in the continuity of Bone
- Fractures can occur in any bone in the body.
- Most bone fractures are caused by falls and accidents.
- Bone fractures caused by disease are referred to as pathological fractures.
- Bone healing is a natural process; treatment revolves around giving the bone optimum conditions to heal.
CLASSIFICATION OF FRACTURE
- OPEN VS CLOSED FRACTURE:
- Open Fracture: An open fracture is also called a compound fracture. In an open fracture, the ends of the broken bone tear the skin causing bone and other internal tissues are exposed, leading higher risk of infection.
- Closed Fracture: A closed fracture is also called a simple fracture. In a closed fracture, the bone is broken without tear in the skin.
- INCOMPLETE VS COMPLETE
- Incomplete Fracture: In an incomplete fracture, the bone doesn’t break completely
- Complete Fracture: In a complete fracture, the bone is broken completely and it is crushed into two or more pieces.
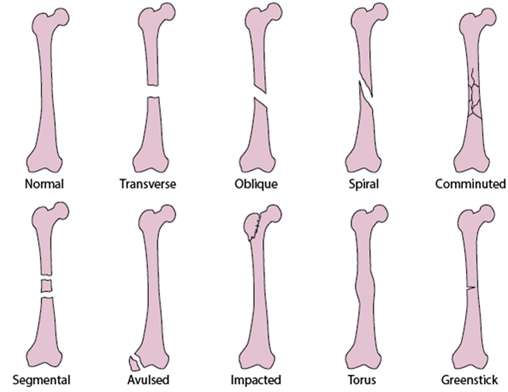
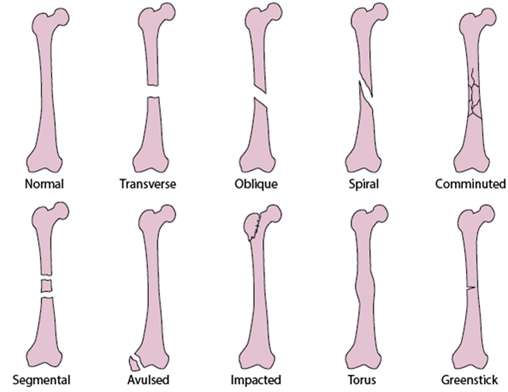
TYPES OF INCOMPLETE FRACTURE
- HAIRLINE FRACTURE:
- This is also known as a stress fracture, is a small crack or severe bruise within a bone.
- This injury is most common in athletes, especially athletes of sports that involve running and jumping.
- GREEN STICK FRACTURE
- The bone partly fractures on one side, but does not break completely because the rest of the bone remains bent.
- This is more common among children, whose bones are softer and more elastic.
- BUCKLE / TORUS FRACTURE
- In which your bone is broken on one side and a bump or raised buckle develops on the other side.
TYPES OF COMPLETE FRACTURE
- SIMPLE FRACTURE
- The bone is broken in one place into two small pieces
- COMMINUTED FRACTURE
- A comminuted fracture is a break or splinter of the bone into more than two fragments.
- A considerable amount of force and energy is exerted causing bone fragmentation
- IMPACTED FRACTURE
- when the bone is fractured, one fragment of bone goes into another
- COMPRESSION FRACTURE
- The bone collapses & breaks under pressure
- DISPLACED FRACTURE
- This involves a displaced fracture fragment that is overriding the other bone fragment. The periosteum is disrupted on both sides
- SEGMENTAL FRACTURE
- In which the bone is broken in two places in a way that leaves at least one segment floating and unattached.
OTHER TYPES OF FRACTURE
- Longitudinal Fracture
- It is a fracture line that runs along the length (Longitudinal axis) of the bone
- Transverse Fracture
- A straight break right across a bone.
- Oblique Fracture
- A fracture that is diagonal to a bone’s long axis
- Spiral Fracture
- A fracture where at least one part of the bone has been twisted
- Intra-articular Fracture
- The break in the bone extends into the surface of a joint
CAUSES OF FRACTURE
- FALLS/ ACCIDENTS: Healthy bones are extremely tough and resilient and can withstand surprisingly powerful impacts. But when this force usually occurs suddenly or is very intense fracture occurs. The strength of the force determines the severity of the fracture
- CHILDREN: Children, who tend to have more physically active lifestyles than adults, are also prone to fractures.
- ADULTS:As people age, two factors make their risk of fractures greater: Weaker bones and a greater risk of falling.
- UNDERLYING ILLNESS/ INFECTION: People with underlying illnesses and conditions that may weaken their bones have a higher risk of fractures. Examples include osteoporosis, infection, or a tumor. As mentioned earlier, this type of fracture is known as a pathological fracture.
- SPORTS INJURIES: Stress fractures, which result from repeated stresses and strains, commonly found among professional sports people, are also common causes of fractures.
PATHOPHYSIOLOGY OF FRACTURE
Due to tensile forces from falls, accidents & injuries leads to break in the continuity of the bone known as fracture
↓
Immediately at the time of fracture, the space between fracture ends is filled with blood-forming a hematoma
↓
Structural and biochemical changes occurs with the influx of inflammatory cells, fibroblasts, chondroblasts and the ingrowth of capillaries forming the primary callus
↓
This primary callus is transformed into a bony callus by the activation of osteo progenitor cells that stabilize the fracture site
↓
Gradual formation of compact cortical bone with greater biomechanical properties and allows for the reduction of the width of the callus leading to bone remodelling
CLINICAL MANIFESTATIONS
- Edema& Swelling:
- Disruption & penetration of bone through the skin or soft tissues or bleeding into the surrounding tissues
- Swelling & edema in a closed space can occlude circulation & cause nerve compression leading to compartment syndrome
- Pain & Tenderness:
- Direct trauma can cause increase pressure on nerves & movement of the fracture parts can lead to muscle injury
- Muscle Spasms:
- Irritation of tissue & spasm occurs as a response to injury & fracture
- Deformity:
- Abnormal posture of extremities as a result of forces of injury & action of muscles pulling the bone fragment into abnormal position.
- Ecchymosis & Contusion:
- Discoloration of the skin as a result of extravasation of blood in subcutaneous tissues
- Loss of Function:
- Disruption of bone or joint prevents functional use of the affected extremity
- Crepitation:
- Grating or crunching of bone fragment producing palpable or audible popping sensation.
PROCESS OF BONE HEALING
- Hematoma Formation
- When fracture occurs bleeding creates a hematoma which surrounds the ends of the bone fragments
- The hematoma is extravasated blood that changes from liquid to semi solid state which occurs in the initial 72 Hours after injury
- Granulation tissue
- During this stage active phagocytosis absorbs the products of local necrosis
- The hematoma converts into granulation tissue consisting of new blood vessels fibroblast & osteoblast that produces during 3-14 days post injury
- Callus Formation
- As minerals like calcium, phosphorus, magnesium and the new bone matrix are deposited in the osteoid, and unorganized network of bone is formed that is woven with fracture cast.
- It usually appears by the second week after injury & can be verified by X-Rays.
- Ossification
- It occurs to prevent movement of the fracture site when the bones are gently stressed
- This occurs from 3 weeks to 6 months after the fracture & continues till the fracture is healed
- At this stage cast can be removed & limited mobility is possible
- Consolidation
- As callus & Ossification continues to develop the distance between the bone fragment is diminishes and eventually the fracture is closed
- Remodeling
- Excess bone tissue is reabsorbed in the final stage of bone healing & bone union is completed
- Gradual return of the injured bone to its pre injury structure, strength and shape occurs.
DIAGNOSTIC EVALUATION
- History & Physical Examination: Collect regarding age, site of fracture, blood supply to area, infection & displacement of fracture
- X-ray: To detect the presence, location & extent of fractured bone
- CT/ MRI: To detect the presence of minor hairline fractures & injury to surrounding tissues.
COMPLICATIONS OF BONE HEALING
- DELAYED UNION: Fracture healing progresses more slowly then expected but healing eventually occurs
- NON-UNION: Fracture fails to heal properly even with treatment resulting in fibrous tissue ossification
- MAL UNION: Fracture heals in expected time but it in a abnormal position leading to deformity of dysfunction
- REFRACTURE: New fracture occurs at the original site
- MYOSITIS OSSIFICANS: Deposition of calcium in the muscle tissue at the site of muscle trauma.
COMPLICATIONS OF FRACTURE
- INFECTION: Open fractures & soft tissue injury have high chance of infection as contaminated tissue is an ideal medium for growth of many pathogens
- COMPARTMENT SYNDROME: It is condition in which elevated pressure at the fracture site causes compression of blood vessels & nerves leading to bleeding, edema and crush injury
- VENOUS THROMBOSIS: The veins of the lower extremities & pelvis are highly susceptible to thrombus formation due to venous stasis caused by application of casts and traction
- FAT EMBOLISM SYNDROME: It is characterized by presence of systemic fat globules from the fracture that is distributed in to the tissues and organs after a traumatic skeletal injury.
MANAGEMENT OF FRACTURE
- FRACTURE REDUCTION: Fracture reduction is fixing the bone or setting the bone after a fracture. The pieces of bone must be put in close proximity to one another so that healing can occur. Fracture reduction is essential to ensure that the bone heals properly and that permanent functional loss or deformity is avoided
- Closed Reduction: Closed Reduction is a non-surgical manual realignment of bone fragments to their previous anatomic position. Traction & counter traction are manually applied to the bone fragments to restore position, length & Alignment. After reduction, traction, casting, external fixation, splints or braces are used to immobilize the injured part to maintain alignment until the fracture is healed
- Open Reduction: Open reduction is the correction of bone through a surgical Incision. It usually includes internal fixation of the fracture with the use of screws, wires, pins, plates, rods & nails.
- FRACTURE IMMOBILIZATION: Immobilization refers to the process of holding a joint or bone in place with a rigid or flexible device. This is done to prevent an injured area from moving and allowing for regular healing of the fractured bone.
PHARMACOLOGICAL MANAGEMENT
- MUSCLE RELAXANTS:
- Carisoprodol, cyclobenzapine, methocarbamol
- To treat pain caused my muscle spasms
- ANTIBIOTICS:
- Cephalosporins like cefazolin
- To prevent infection in open fractures
- SUPPLEMENTS:
- Calcium & Vitamin C supplements
- To promote bone & muscle healing.
NUTRITIONAL THERAPY
- Nutrition must include adequate proteins (1gm/kg body weight), vitamins especially B,C &D, minerals like calcium, phosphorous & magnesium to ensure bone & tissue healing
- Well balanced diet of 3 meals per day is advised for healing
- Adequate fluid Intake of 2000-3000 ml/ day to promote bladder & bowel function
- High fiber diet like fruits & vegetables to prevent constipation
- If client has signs of cramping & abdominal pressure due to immobilization then advice to eat small & frequent meals of 6 times a day rather than eating full meals.
SURGICAL MANAGEMENT
- OPEN REDUCTION & INTERNAL FIXATION (ORIF):
- Open reduction and internal fixation (ORIF) is surgery to repair a broken bone. Open reduction means to make an incision to reach the bones & move them back into their normal position.
- Internal fixation means metal screws, plates, sutures, or rods are placed on the bone to keep it in place while bone healing takes place
- SURGICAL DEBRIDEMENT & IRRIGATION OF OPEN FRACTURE:
- The most important initial step in the surgical wound management of open fractures is regarded as copious fluid irrigation along with meticulous debridement of surrounding contaminated soft tissues.
- Wound irrigation to remove debris and lessen bacterial contamination is an essential component of open fracture care when performed properly; wound irrigation can enhance wound healing by reducing infection and its related morbidities.
- Isotonic saline is regarded as the most appropriate and preferred irrigant because it is a nontoxic solution that does not damage the healing tissue.
NURSING ASSESSMENT
- Assess the fractured site for the neurovascular status like colour, temperature, capillary refill time, peripheral pulses &Edema distal to the Injured Extremity
- Colour may be pink, pale or cyanotic and temperature can be hot, warm, cool or clammy in the fractured extremity
- Pallor or cool Extremity indicates Arterial Insufficiency
- Warn , cyanotic extremity indicates poor venous return
- Capillary Refill (Blanching of the nail bed) is assessed to identify the return of blood in the nail bed, when compressed within 2-3 seconds
- Pulses on both the unaffected and injured extremity are compared to identify the difference in rate and Quality. Pulse is also measured using an audible Doppler device
- Diminished or Absent Pulse indicates Vascular dysfunction or Insufficiency
- Range of Motion of the Affected Extremity is assessed to Identify nerve Injury
- Assess the Sensory and Motor Function of the Affected Extremity
- Reduced Motion or Strength on the affected Extremity indicates Neuronal damage
- Sensation like Paraesthesia (Numbness & Tingling) or Paresis and Paralysis indicates Nerve Impairment
- Monitor the Vital Signs, ECG, Oxygen Saturation to identify the hemodynamic Status and potential complications
- Assess the location, Quality and Intensity of Pain by using Pain Scale
NURSING MANAGEMENT:
- Frequent Assessment of the Neurovascular status and Vital Signs
- Monitor the Injured Site for bleeding, tenderness, swelling & limitations in Movement
- Educate on the type of Immobilization and assistive devices required
- Provide Assurance that pain Medications will be given to relieve pain
- If Surgical Intervention is required, Prepare the client for Surgery by obtaining written consent from the client or the Significant caregivers
- Identify the limitations of activity and precautions to be followed while providing care and support the Injured Extremity
- Strict Asepsis should be carried out, when giving care to Surgical Clients
- Wound dressing and wound drainage should be monitored every hour and documented accurately for surgical clients
- Fluids are administered around 2500ml/day to prevent Dehydration and Constipation
- Provide Nutrition rich in Protein, Calcium, Vitamins and Roughage like high fibres, vegetables, Fruits, meat etc.
- Judicial use of Analgesics is Indicated to relieve Pain
- Administer Antibiotics and Supplements as prescribed by the Physician
- Administer Stool Softeners and laxatives to prevent constipation
- Provide all bed side Nursing care measures until Recovery
- Gradually Assist in Range of Motion and Exercises as recommended to prevent Spasticity of the Extremities and aid in Movement
- Evaluate the Prognosis of the client and prepare for Discharge once the Fracture is healed
Thank you